Vagus Nerve Injury
 The vagus nerve is the 10th cranial nerve. Its primary responsibility is to provide parasympathetic innervation to organs in the chest and abdomen, and separately, it gives rise to the recurrent laryngeal n. which provides innervatrion to the larynx for airway and speech control. The overall published incidence of all cranial nerve injuries after carotid endarterectomy ranges from 11%-14%, however these injuries are almost always temporary. The vagus nerve is the second most common cranial nerve to be injured during this procedure with an incidence of 4%.
The vagus nerve is the 10th cranial nerve. Its primary responsibility is to provide parasympathetic innervation to organs in the chest and abdomen, and separately, it gives rise to the recurrent laryngeal n. which provides innervatrion to the larynx for airway and speech control. The overall published incidence of all cranial nerve injuries after carotid endarterectomy ranges from 11%-14%, however these injuries are almost always temporary. The vagus nerve is the second most common cranial nerve to be injured during this procedure with an incidence of 4%.
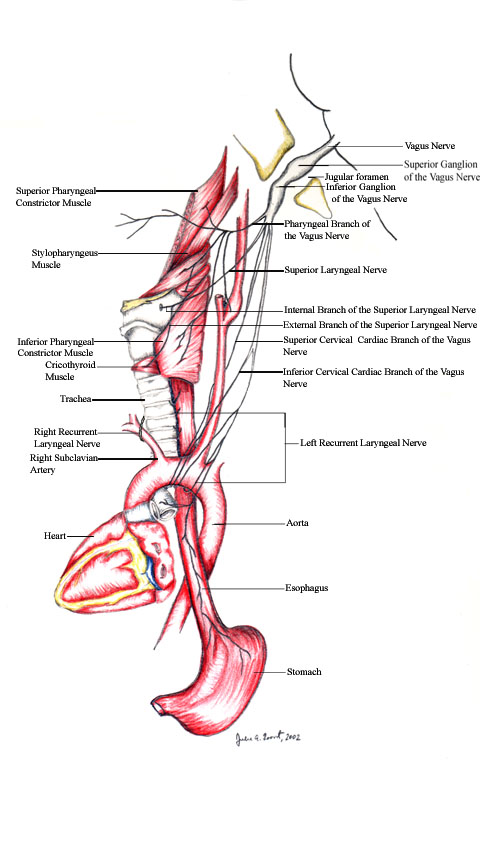
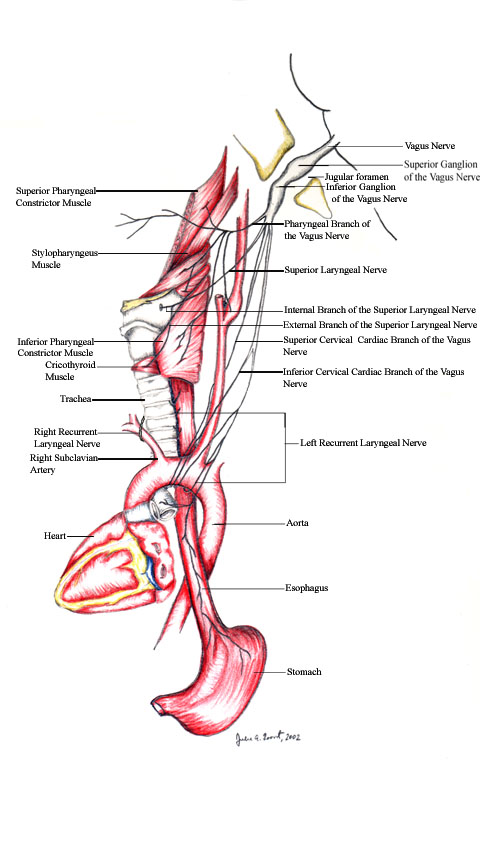
It originates at the medulla just below the glossopharyngeal nerve. It then exits the skull via the jugular foramen together with the glossopharyngeal nerve and the spinal accessory nerve. The vagus nerve immediately forms the ganglion nodosum at which point the superior laryngeal nerve comes off. This nerve then divides into an internal branch which provides sensation to the epiglottis and the larynx above the vocal cords and an external branch which provides the motor innervation to the cricothyroid muscle and the inferior pharyngeal constrictor. These branches of the vagus nerve are rarely damaged unless complete mobilization of the carotid bifurcation is necessary. Injury to the superior laryngeal nerve leads to hoarseness and dysphagia.
The vagus nerve then continues its course posterolateral to the carotid artery and jugular vein into the neck in the carotid sheath. At the root of the neck, the right recurrent laryngeal nerve arises from the vagus trunk and loops around the right subclavian artery. The left recurrent laryngeal nerve has a different path as it arises from the trunk of the vagus nerve in the mediastinum and loops around the aortic arch at the level of the ligamentum arteriosum. Despite their varied initial course, both the right and the left nerves ascend in the neck behind the common carotid artery in the groove between the trachea and the esophagus. The recurrent laryngeal nerves are responsible for innervating the intrinsic muscles of the larynx that control the vocal cord on the ipsilateral side. Injury to this nerve therefore results in paralysis of the vocal cord on the damaged side. Once again, this nerve is seldom exposed during carotid endarterectomy and is usually damaged by traction or cautery. To note, bilateral recurrent laryngeal nerve injury is a serious complication that can lead to a compromised airway due to unopposed vocal cords in the midline. Due to the possibility of this serious complication, many recommend indirect laryngoscopy before the second stage of bilateral staged carotid endarterectomies.
Overall, injury to the main trunk of the vagus nerve is rare. It may be injured in high exposure and by careless use of the cautery. Given that vagus nerve injury from a carotid endarterecotomy can be debilitating complication avoidance by careful dissection, early recognition, and immediate correction of these injuries are important in the management of this complication.
- Driscoll, Peter J. MBBS, BSc, MRCS(Ed): Chalmer, Roderick T.A. MD, FRCS. The use of a nerve stimulator in a difficult carotid surgery. Journal of Vascular Surgery. March 2002.
- Schauber, Michael D. Maj., USAF, MC, FS; Cranial/cervical nerve dysfunction after carotid endarterectomy. Journal of Vascular Surgery. March 1997.
- Schauber, Michael D. Maj., USAF, MC, FS; Cranial/cervical nerve dysfunction after carotid endarterectomy. Journal of Vascular Surgery. March 1997.
- AbuRahma AF, Lim RY. Management of vagus nerve injury after carotid endarterectomy. Surgery. March 1996.
 The vagus nerve is the 10th cranial nerve. Its primary responsibility is to provide parasympathetic innervation to organs in the chest and abdomen, and separately, it gives rise to the recurrent laryngeal n. which provides innervatrion to the larynx for airway and speech control. The overall published incidence of all cranial nerve injuries after carotid endarterectomy ranges from 11%-14%, however these injuries are almost always temporary. The vagus nerve is the second most common cranial nerve to be injured during this procedure with an incidence of 4%.
The vagus nerve is the 10th cranial nerve. Its primary responsibility is to provide parasympathetic innervation to organs in the chest and abdomen, and separately, it gives rise to the recurrent laryngeal n. which provides innervatrion to the larynx for airway and speech control. The overall published incidence of all cranial nerve injuries after carotid endarterectomy ranges from 11%-14%, however these injuries are almost always temporary. The vagus nerve is the second most common cranial nerve to be injured during this procedure with an incidence of 4%.